Unveil the Hidden Causes of Varicose Veins for Permanent Treatment Results
February 19, 2026
This article explores a minimally invasive method for treating varicose veins known as Clarivein treatment. It outlines the main advantages of this technique. It also explains the mechanism of action in clear clinical terms. In addition, it compares the method with other treatments such as sclerotherapy. Together, these points give readers essential insights into how this approach works.
The primary goal is to eliminate venous reflux. Medical research (from The Whiteley Clinic) now clearly shows that vein stripping no longer serves as a viable option because neovascularisation causes the long-term recurrence of varicose veins. Thermal ablation aims to induce transmural death by destroying the entire vein wall rather than merely damaging the endothelium. When only the endothelium suffers damage, thrombosis may occur, but the vein wall remains intact, allowing potential recanalisation. This concept holds particular importance in large-diameter veins treated with chemical sclerotherapy, where the problem lies not in the diameter itself but in the depth of the vein wall. Data demonstrate that ablating the vein wall results in immediate vein closure in over 99% of cases at 1 year, with 88% closure at 15 years, and no complete failures.
The main challenge in thermal ablation arises from the need to administer tumescent anaesthesia around the target vein. Some companies assert that using lower power settings can eliminate the need for anaesthesia. However, this is only the case because the damage to the vein wall is insufficient. As a result, sensory nerves in the surrounding tissues are not activated, meaning the patient experiences no pain. Unfortunately, this lack of pain simply indicates that the treatment has been inadequate, and the risk of recurrence is very high. This emphasises the importance of evaluating treatments scientifically before accepting commercial claims. Therefore, if thermal ablation is performed without the use of local anaesthetic and the patient reports no discomfort, it is likely that the procedure was inadequate.
A key advantage of Clarivein treatment, and similarly with glue techniques, is that they can be performed without tumescent anaesthesia. However, a non-anaesthetic technique had already been available: foam sclerotherapy. Unfortunately, foam sclerotherapy is not particularly successful in saphenous veins (or “truncal veins”), which are the veins that are treated by Clarivein , unless specific techniques are used to prevent foam dispersion or dilution. Without such measures, success rates are inferior to modern endovenous thermal techniques and often require repeated interventions.
Foam sclerotherapy has demonstrated notably better results in smaller veins. Although vein diameter is not the primary concern, it can be measured via ultrasound. The critical factor is wall thickness, as this determines the extent of tissue destruction. In venous malformations with thin walls, outcomes are excellent even in veins measuring 20–30 mm in diameter, due to the reduced presence of smooth muscle cells in the media. In contrast, the Great Saphenous Vein (GSV) and Small Saphenous Vein (SSV) possess significantly thicker walls, which influence treatment outcomes. This explains why thinner-walled veins respond better to foam sclerotherapy. Studies have also shown that Sodium Tetradecyl Sulphate (STS) penetrates deeper than Polidocanol. Whilst Clarivein treatment in the US is often performed using Polidocanol, STS is now being used by many doctors in liquid form with the same technique. 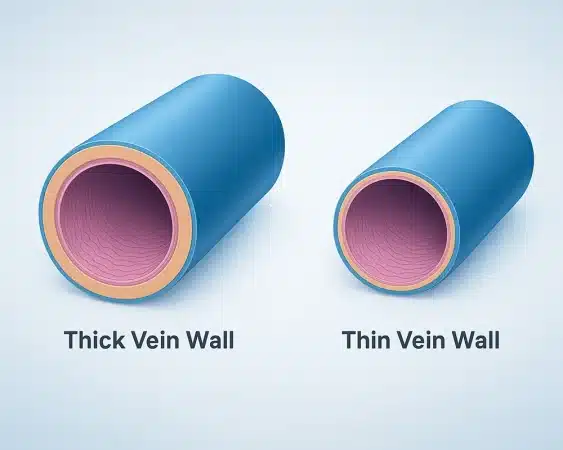
Before performing any technique on a patient, clinicians must thoroughly understand its mechanism of action, both in vitro and in vivo. Simply damaging the endothelium is likely to be insufficient. If the media layer remains unaffected and fibrosis does not develop adequately, patients face a high risk of vein recanalisation and thrombosis. Regarding Clarivein treatment and MOCA (mechanochemical ablation) technology, most current data focus on clinical outcomes. However, researchers need a deeper understanding to explainthe claimed 97% success rate, especially since foam sclerotherapy does not show similar results.
The investigation must examine the cellular and tissue levels. Researchers know that Clarivein treatment causes tissue destruction, as shown by the debris collected on the catheter wire. This effect goes beyond simple thrombosis. In a German study, clinicians treated GSVs in five patients using Clarivein treatment, then removed vein segments and examined them under a microscope. They found significant endothelial damage in most areas, but mechanical damage did not extend beyond that. However, research performed at The Whiteley Clinic challenged this, with their research suggesting that the rotating wire at the end of the Clarivein does disrupt the vein wall, forcing the sclerotherapy solution deeper into the vein wall.
The following video shows Prof Mark Whiteley presenting at an international conference in April 2013:
Performing a duplex ultrasound before selecting any treatment option ensures choosing the most suitable method for the patient. At The Whiteley Clinic, clinicians conduct thorough consultations prior to any intervention, and after the necessary assessments, the most effective treatment will be offered.