Unveil the Hidden Causes of Varicose Veins for Permanent Treatment Results
February 19, 2026
PUBLISHED BY
Primary avalvular varicose anomalies are a naturally occurring phenomenon that might be misdiagnosed as neovascular tissue in recurrent varicose veins
From the The Whiteley Clinica; and the Faculty of Health and Biomedical Sciences, University of Surrey.b
Author conflict of interest: none.
Presented as a poster at the American Venous Forum, 26th Annual Meeting, New Orleans – February 2014
Charing Cross International Symposium, London – April 2014
Sociedade Portuguesa de Cirurgia Cardio- Toracica e Vascular (SPCCTV), Algarve, Portugal – November 2014
VEITH Symposium™, New York – November 2014
Presented as ‘PAVA – More Understanding of Peri-Adventitial Venous Abnormalities’
The objective of this study was to report a phenomenon in some patients with primary varicose veins that resembles neovascular tissue in postsurgical recurrences – primary avalvular varicose anomalies (PAVA).
Between March 2012 and July 2013, 756 patients (122 men, 634 women) with primary varicose veins (mean age, 53 years; range, 18-89 years) underwent duplex ultrasonography with retrospective analysis of their reflux patterns.
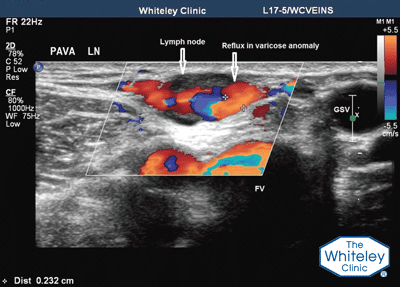
We diagnose PAVA as small, refluxing vessels in legs with primary varicose veins and no history of surgery, trauma, or infection in the area that show one or more of three patterns of distribution: lymph node pattern – PAVA arising directly from groin lymph nodes; peritruncal pattern – PAVA wrapping around the great, small, or anterior accessory saphenous veins; and atypical pattern. PAVA are predominantly found within the saphenous fascia, but components have been found to emerge into the superficial and deep venous compartments.
We analyzed results from 1398 legs (756 patients). Sixty-four legs (4.6%) in 58 patients exhibited PAVA, bilateral in six patients and unilateral in 52 patients. Lymph node involvement and peritruncal PAVA were seen in 23.4% and 70.3% of legs, respectively. The small saphenous vein was the most common truncal vein to be involved (48.9% of peritruncal cases). More than one pattern of PAVA could be observed in seven legs. Of the 48 women with PAVA, 42% had concurrent pelvic vein reflux.
Neovascularization has been identified as a major cause of clinically recurrent varicose veins after open surgery (‘stripping’). Neovascular tissue has also been described after endovenous thermoablation.
We suggest that this is probably incorrect and might represent PAVA undetected preoperatively in some cases. PAVA are thinwalled, serpiginous, incompetent vessels that resemble neovascular tissue. We conclude that neovascularization should be diagnosed as a source of recurrence after endovenous surgery only if PAVA had been actively looked for, and excluded, in the preoperative diagnostic duplex ultrasound examination. (J Vasc Surg: Venous and Lym Dis 2014;2:390-6.)
PAVA was discovered by the vascular technologists at the The Whiteley Clinic and so every Whiteley clinic vascular technologist is trained to look for PAVA and to note exactly where it is and how extensive it is.
All The Whiteley Clinic patients have their PAVA treated as part of their bespoke varicose vein treatment under The Whiteley Protocol®, reducing yet another cause of recurrent varicose veins in the future.
Alexandra E Ostler (The Whiteley Clinic Summer Research Fellow 2013 & Medical Student)
Judith ‘Judy’ M Holdstock (Chief Vascular Technologist, The Whiteley Clinic)
Charmaine ‘Charlie’ C Harrison (Senior Vascular Technologist, The Whiteley Clinic)
Timothy J Fernandez-Hart (Vascular Technologist, The Whiteley Clinic)
Journal of Vascular Surgery: Venous and Lymphatic Disorders Journal of Vascular Surgery: Venous and Lymphatic Disorders 2014:Vol 2(4);390–396 http://dx.doi.org/10.1016/j.jvsv.2014.05.003
American Venous Forum, 26th Annual Meeting, New Orleans – February 2014 (poster)
Charing Cross International Symposium, London – April 2014
Sociedade Portuguesa de Cirurgia Cardio-Toracica e Vascular (SPCCTV, Algarve, Portugal – November 2014
VEITH Symposium™, New York – November 2014. Presented as ‘PAVA – More Understanding of Peri-Adventitial Venous Abnormalities’
Duplex ultrasound showing PAVA (primary avalvular varicose anomalies) – red and blue colours show blood flow in the veins. PAVA first described in 2014 by the The Whiteley Clinic
After any trauma of the veins in the leg, including the old high saphenous tie and stripping type operation for varicose veins, the body grows back lots of tiny new veins. These are called ‘Neovascular’ vessels or ‘new veins’. Unfortunately they never have valves and so always cause recurrence of the varicose vein reflux.
For many years we have been noticing patients with lots of little veins around their major veins, which look as if they are neovascular vessels. These patients deny having had any trauma or operations to their veins, and previously these have been ignored.
We have previously shown that endovenous techniques used by the Whiteley Protocol do not cause neovascularisation and the growth of these new vessels. However, some other surgeons have reported neovascularisation found after endovenous laser ablation.
In this study, we showed that almost 5% of normal people who have never had any trauma or surgery to their veins and their legs, have PAVA at their initial scan.
In this study we pointed out it is essential that PAVA is found and noted on the 1st diagnostic duplex ultrasound scan for 2 reasons:
Before the The Whiteley Clinic discovered PAVA, researchers from other academic units had reported that neovascularisation can occur after endovenous laser ablation. However, it cannot, as long as it is done properly. They had merely mistaken this naturally occurring phenomenon as a cause of recurrent venous reflux after endovenous laser ablation, as they had not looked for this preoperatively!